Perimenopause Awareness Month - Let's Get the Conversation Started!
Understanding Menopause:
The Transition from Perimenopause
Perimenopause marks a significant transition in a woman’s life, bridging the fertile years to the end of the menstrual cycle. This natural phase can evoke a complex blend of emotions and physical changes as hormonal fluctuations become more pronounced. Understanding perimenopause is crucial for navigating the challenges that come with it, allowing for better health management during this pivotal time.
Understanding the Perimenopause Transition
Perimenopause is the crucial period leading up to menopause, marked by a gradual decline in ovarian function and hormone production, particularly estrogen. This shift can result in a myriad of changes, both physically and emotionally, as your body adjusts to fluctuating hormone levels. While some women might begin this transition in their mid-30s, most will notice changes in their mid-40s. It's during this time that menstrual cycles can become unpredictable, often accompanied by symptoms such as hot flashes, mood swings, and changes in sexual drive. These changes are natural, though they can sometimes be disruptive.
Understanding this transition helps in recognizing that these symptoms are part of a natural process rather than isolated health issues. By staying informed, women can take proactive steps to manage their symptoms, such as lifestyle adjustments or consulting healthcare providers for tailored treatments. It's also important to acknowledge that perimenopause varies greatly from person to person—what one woman experiences can be entirely different from another's journey. This variability underscores the importance of personalized care and self-awareness during this significant phase of life.
Hormonal Changes During Perimenopause
During perimenopause, the most significant hormonal change is the decline in estrogen production by the ovaries. Estrogen is crucial for regulating the menstrual cycle and maintaining various body functions, including bone density, skin elasticity, and mood stability. As its levels wane, women often experience a cascade of symptoms, such as irregular periods, hot flashes, and night sweats.
Progesterone, another key hormone, also fluctuates during this period. The imbalance between estrogen and progesterone can lead to heavier or lighter menstrual bleeding and exacerbate symptoms like mood swings and sleep disturbances.
These hormonal shifts can also affect the skin, leading to increased dryness and a more pronounced appearance of fine lines and wrinkles. In some cases, women might notice changes in hair texture or even thinning hair.
The body’s metabolism tends to slow down as well, contributing to weight gain and a shift in body fat distribution. This is why maintaining a healthy diet and exercise regimen becomes even more critical.
Understanding these hormonal changes helps in anticipating the physical and emotional symptoms that may arise, making it easier to manage them effectively.
Typical Age for Perimenopause to Start
The onset of perimenopause is highly individual, with most women beginning to notice signs between the ages of 40 and 45. However, it's not uncommon for some to experience symptoms as early as their mid-30s or as late as their mid-50s. This variability can be influenced by factors such as genetics, lifestyle choices, and overall health. For instance, women with a family history of early menopause might find themselves entering this phase sooner than their peers. Additionally, lifestyle factors such as smoking or high-stress levels can accelerate the onset.
It's essential to pay attention to your body’s signals during this period. Menstrual cycles may start to become erratic, with periods that are irregular or vary in intensity. Such changes serve as early indicators that perimenopause is beginning. Given the broad age range during which perimenopause can start, staying attuned to these signs can help you prepare and seek appropriate guidance or treatment.
Engaging in a proactive dialogue with your healthcare provider can provide valuable insights tailored to your unique situation. They can help differentiate between typical perimenopausal symptoms and other potential health issues that might require attention. Recognizing the age-related onset of perimenopause allows for better planning and management of symptoms, ensuring a smoother transition through this natural phase of life.
Duration of Perimenopause
Perimenopause varies significantly in duration from one woman to another. On average, this transitional phase lasts about four years, but it can extend up to eight years or be as brief as a few months. The length of perimenopause can be influenced by multiple factors, including genetics, overall health, and lifestyle choices. Women with a family history of early menopause may experience a longer perimenopausal phase, while those maintaining a healthy lifestyle may find their symptoms more manageable and their transition period shorter.
During this time, the ovaries gradually produce less estrogen, leading to the array of symptoms commonly associated with perimenopause. These hormonal fluctuations can make predicting the end of perimenopause challenging. It's a highly individualized process, with some women experiencing only mild, short-term symptoms and others undergoing more prolonged, intense changes.
Understanding that the duration of perimenopause can vary widely helps in setting realistic expectations. Tracking your symptoms and menstrual cycle can provide valuable insights into how your body is navigating this transition. Communicating these observations with your healthcare provider can aid in developing personalized strategies to manage symptoms effectively. Whether your perimenopause phase is fleeting or extended, staying informed and proactive can help you maintain a sense of control and well-being during this significant life stage.
Identifying Perimenopause Symptoms
Perimenopause presents a variety of symptoms, many of which can be quite distinct from your usual experiences. One of the earliest signs is often an irregular menstrual cycle. You might find your periods becoming erratic, with cycles that are longer, shorter, or missing altogether. This irregularity can be accompanied by other common symptoms such as hot flashes, which feel like sudden waves of heat sweeping over your body, often leading to sweating and
flushed skin.
Another significant symptom to be aware of is mood swings. Hormonal fluctuations can cause sudden changes in emotional states, leading to irritability, anxiety, or even bouts of depression. You may also notice a decline in libido, which can affect your interest in sexual activities. Vaginal dryness is another common issue, causing discomfort during intercourse and sometimes even daily activities.
Sleep disturbances are frequently reported, with many experiencing night sweats that can disrupt rest. Insomnia or difficulty staying asleep can leave you feeling fatigued and irritable throughout the day. Additionally, some women report a need to urinate more frequently or urgently, which can be particularly inconvenient.
Keep an eye on any changes in your overall health and well-being. For example, you might experience weight gain or find it harder to maintain your usual weight. This is often due to the slowing metabolism associated with hormonal changes. Paying attention to these symptoms can help you better understand what your body is going through, making it easier to seek appropriate care and manage your health during this transition.
Symptoms and Causes of Perimenopause
As estrogen levels start to wane, perimenopause ushers in a host of symptoms that can affect daily life. Irregular periods are often the first clue, but many women also contend with hot flashes that seem to strike out of nowhere, turning routine moments into sweaty ordeals. Night sweats are another common companion, disrupting sleep and leaving you feeling exhausted by morning. Mood swings can make even the most composed individuals feel like they’re on an emotional rollercoaster, contributing to irritability, anxiety, and sometimes depression. These emotional shifts can be particularly challenging, as they might not align with external stressors, making them feel even more bewildering.
Vaginal dryness is another symptom that doesn’t get enough attention but can significantly impact your comfort and sexual health. This can make intimacy less enjoyable and sometimes even painful. Additionally, many women notice a decrease in their libido, which can be distressing and add strain to personal relationships. Insomnia or other sleep disturbances often follow, further exacerbating mood issues and overall fatigue.
Weight gain is another unwelcome guest during this phase. The slowing of metabolism caused by hormonal changes can make it harder to maintain your usual weight, often leading to changes in body composition. Understanding these symptoms and their hormonal underpinnings can be empowering, enabling you to seek appropriate medical advice and lifestyle adjustments to manage this significant phase more effectively.
Perimenopause Anxiety and Mental Health
Hormonal fluctuations during perimenopause can significantly affect mental health, often leading to heightened anxiety or depressive symptoms. As estrogen levels decline, the brain's neurotransmitter balance can be disrupted, resulting in feelings of unease or persistent worry. These emotional changes can be particularly disorienting, as they may arise independently of external stressors, making it difficult to pinpoint a specific cause.
Symptoms of perimenopausal anxiety can manifest physically, too, with women experiencing increased heart rate, sweating, or muscle tension. These physiological responses can further exacerbate feelings of anxiety, creating a feedback loop that amplifies distress. Additionally, the sleep disturbances often associated with perimenopause, such as insomnia or night sweats, can contribute to a heightened sense of anxiety, making it challenging to maintain emotional equilibrium.
Mood swings are another common experience during perimenopause. Rapid shifts in mood can be unsettling, leading to irritability, frustration, or even bouts of unexplained sadness. This emotional volatility can impact personal relationships and overall quality of life, adding another layer of complexity to this transitional phase.
Seeking support from healthcare providers is crucial. They can offer a range of interventions, from lifestyle modifications to medication, to help manage these mental health challenges. Cognitive-behavioral therapy (CBT) and mindfulness techniques can also be effective in mitigating anxiety symptoms, providing strategies to cope with emotional turbulence. By addressing both the physiological and psychological aspects of perimenopause, women can find a balanced approach to navigating this challenging but natural life stage.
Changes in Menstrual Cycles During Perimenopause
During perimenopause, the menstrual cycle can become unpredictable due to hormonal fluctuations. You might notice your periods becoming erratic, with cycles that are either longer or shorter than what you're used to. Bleeding may also vary, with some months being significantly heavier or lighter than others. Such changes are a direct result of your ovaries producing less estrogen, causing a ripple effect on your menstrual cycle. It's not uncommon for some women to experience spotting between periods or to skip periods altogether for a few months before they resume. These variations in menstrual patterns can sometimes make it challenging to predict your cycle, which can add a layer of stress to your daily routine. Alongside these changes, you may also observe a shift in premenstrual symptoms; cramps, bloating, and mood swings might feel more intense or, conversely, less noticeable. It's essential to track these changes, as they provide valuable insight into how your body is transitioning. Keeping a journal of your menstrual cycle, including flow intensity and any accompanying symptoms, can help you communicate more effectively with your healthcare provider. This detailed record will be instrumental in developing a personalized plan to manage your perimenopausal symptoms more effectively.
Managing Perimenopause Symptoms
Navigating perimenopause effectively hinges on managing its diverse symptoms. Begin by prioritizing a balanced diet rich in fruits, vegetables, whole grains, lean protein, and healthy fats to combat weight gain and support overall health. Exercise regularly, incorporating both cardio and weight-bearing activities, to maintain bone density, improve mood, and enhance sleep quality. Staying physically active can also alleviate some of the anxiety and depression associated with hormonal changes.
Hydration is crucial—drink plenty of water to help manage symptoms like hot flashes and vaginal dryness. Additionally, dressing in layers and keeping your living spaces cool can mitigate the discomfort of sudden hot flashes. Incorporate stress-relief practices such as meditation, deep-breathing exercises, or yoga to help manage mood swings and improve mental clarity.
Limiting caffeine and alcohol can also make a significant difference, as both can exacerbate symptoms like hot flashes and disrupt sleep patterns. Tobacco use should be avoided due to its negative impact on hormone levels and overall health. Over-the-counter remedies, such as vaginal lubricants, can address specific issues like vaginal dryness, enhancing comfort during sexual activity.
For those experiencing severe symptoms, consulting a healthcare provider about hormone replacement therapy (HRT) or other medications might be beneficial. They can tailor a treatment plan to your specific needs, improving your quality of life during this transition.
Lifestyle Changes for Symptom Management
Adopting healthy lifestyle habits can play a pivotal role in managing the array of symptoms that accompany perimenopause. Start by focusing on a nutrient-dense diet rich in colorful fruits, vegetables, lean proteins, and whole grains to support overall well-being and help mitigate weight gain. Regular physical activity, including both cardiovascular exercises like brisk walking or cycling and weight-bearing exercises such as strength training, is essential for maintaining bone density and boosting mood.
Adequate hydration is key, so aim to drink plenty of water throughout the day, which can help alleviate symptoms like hot flashes and vaginal dryness. Creating a cool, comfortable sleeping environment and dressing in layers can also offer relief from sudden temperature changes. Incorporating stress management techniques, such as meditation, deep breathing exercises, or yoga, can help stabilize mood swings and improve mental clarity.
It's wise to limit or avoid substances that can worsen symptoms. Reduce caffeine and alcohol intake, as both can exacerbate hot flashes and disrupt sleep. If you smoke, consider quitting; smoking can not only lead to an earlier onset of menopause but also intensify symptoms. Engaging in these lifestyle changes not only helps in managing perimenopausal symptoms but also enhances overall health, setting a strong foundation for well-being during this transitional period.
Factors That Worsen Perimenopause Symptoms
Certain lifestyle habits can significantly exacerbate perimenopause symptoms, making this transitional phase more challenging. A diet high in sugary foods, processed snacks, and saturated fats can amplify weight gain, hot flashes, and mood swings. Alcohol and caffeine are notorious for worsening symptoms like night sweats and insomnia, disrupting your sleep patterns and overall well-being.
Inactivity is another culprit. A sedentary lifestyle can lead to weight gain, increased stress levels, and reduced bone density, all of which can intensify perimenopause symptoms. Regular physical activity is essential for maintaining not only physical health but also mental clarity and emotional stability.
Smoking is particularly detrimental during perimenopause. Not only does it accelerate the onset of menopause, but it also heightens the severity of symptoms such as hot flashes and vaginal dryness. Additionally, smoking impacts bone density, increasing the risk of osteoporosis.
Chronic stress can act as a magnifying glass, intensifying every symptom. Elevated stress levels can disrupt sleep, exacerbate mood swings, and weaken your immune system. Incorporating stress management techniques such as meditation, deep breathing, or yoga can help mitigate these effects.
Finally, inadequate sleep hygiene can lead to a vicious cycle of fatigue and irritability, worsening mood swings and cognitive difficulties. Adopting good sleep practices, such as maintaining a consistent bedtime routine and creating a restful environment, is crucial for alleviating perimenopause symptoms.
Early Onset Perimenopause
For some women, perimenopause can begin earlier than the typical mid-40s, sometimes starting in their mid-30s or even earlier. Factors contributing to early onset include genetics, lifestyle choices, and certain medical treatments like chemotherapy or radiation. Women who smoke are also at higher risk for experiencing perimenopause earlier than their non-smoking peers. Additionally, surgical procedures such as hysterectomy or oophorectomy can trigger early perimenopause. It's essential to stay vigilant for signs like irregular menstrual cycles, mood swings, or hot flashes if you fall into these risk categories. Early onset perimenopause can bring a unique set of challenges, but being aware of these factors allows for timely interventions and adjustments in lifestyle or treatment options.
Health Risks Associated with Perimenopause
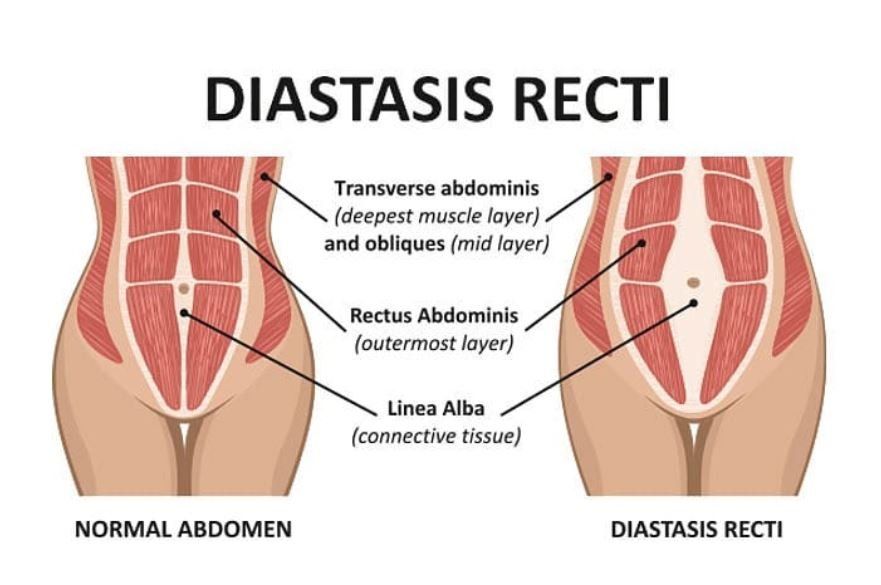
As women transition through perimenopause, the decline in estrogen can lead to several health risks that warrant attention. One significant concern is the increased risk of osteoporosis. Estrogen plays a crucial role in maintaining bone density, and its reduction can result in bones becoming more brittle and susceptible to fractures. This makes weight-bearing exercises and a diet rich in calcium and vitamin D more critical than ever.
Cardiovascular health is another area that may be affected during perimenopause. Lower estrogen levels can influence the heart and blood vessels, potentially increasing the risk of heart disease. Monitoring cholesterol levels, maintaining a healthy weight, and engaging in regular physical activity are vital steps to mitigate these risks.
Additionally, some women may experience changes in their skin, such as increased dryness and a loss of elasticity, leading to more pronounced fine lines and wrinkles. This is due to the decreased estrogen levels affecting collagen production. Moisturizers, hydration, and a balanced diet can help manage these skin changes.
Urinary issues can also arise, such as increased urgency or frequency, which may be related to changes in the urinary tract. Pelvic floor exercises can help strengthen the muscles in this area, providing some relief.
Mental health is another critical aspect to consider. The hormonal shifts can exacerbate feelings of anxiety, depression, and mood swings. Addressing these issues with a healthcare provider is essential, as they can offer tailored strategies for mental well-being, including therapy or medication if needed.
Being aware of these potential health risks allows women to take proactive steps to safeguard their well-being during this transitional period.
Pregnancy During Perimenopause
Even during perimenopause, the possibility of pregnancy remains. While menstrual cycles may become irregular, ovulation can still occur unpredictably. This unpredictability can lead to unexpected pregnancies if effective contraception is not used. For women who wish to avoid pregnancy, it is crucial to continue using reliable birth control methods until a healthcare provider confirms that menopause has been reached. This typically means no menstrual cycles for 12 consecutive months.
Join in on the perimenopause conversation with Dr. Mantor's Wrinkle and Weight Solutions, LLC in the conversation as we observe #NationalPerimenopauseMonth.
Send us your questions regarding perimenopause and menopause and if your question is one we address, on our Facebook and Instagram channels, you will receive a $50 Mantor Money gift card! Please email your questions to: KristinwithDrMantor@gmail.com
Helpful links:
https://menopause.org/
https://menopauseassociation.org/
https://nationalmenopausefoundation.org/
https:https://menopauseassociation.org///menopause.org/